
Reducing Clinician Burnout Through Smarter Documentation With Reteta
Reducing Clinician Burnout Through Smarter Documentation With Reteta
Featured Image


The clinic day ends, but the work doesn’t. Many clinicians head home only to face another round of typing notes, coding visits, and making sure every box in the Electronic Health Record (EHR) is filled correctly. This “pajama time” of after-hours charting has become the silent weight of modern healthcare, eating into evenings, weekends, and family life.
It’s not just tiring, it’s one of the biggest drivers of burnout. And the root of this burden lies in the way documentation is handled. The path forward lies in rethinking documentation - transforming it from a source of fatigue into a driver of efficiency, balance, and sustainable outcomes.
The Documentation Dilemma
Electronic Health Records were designed to simplify care delivery, but the reality has often been the opposite. Clinicians spend hours entering details, toggling between templates, and assigning codes manually. Add compliance checks and the pressure to avoid denials, and what should be seamless becomes a daily uphill climb.
This dilemma isn’t about poor time management, it’s about a system where administrative tasks dominate clinical ones. According to the AMA, physicians spend nearly two hours on EHR and desk work for every hour of direct patient care. That imbalance drains energy, steals focus, and shifts attention away from the very reason clinicians entered medicine: caring for patients.
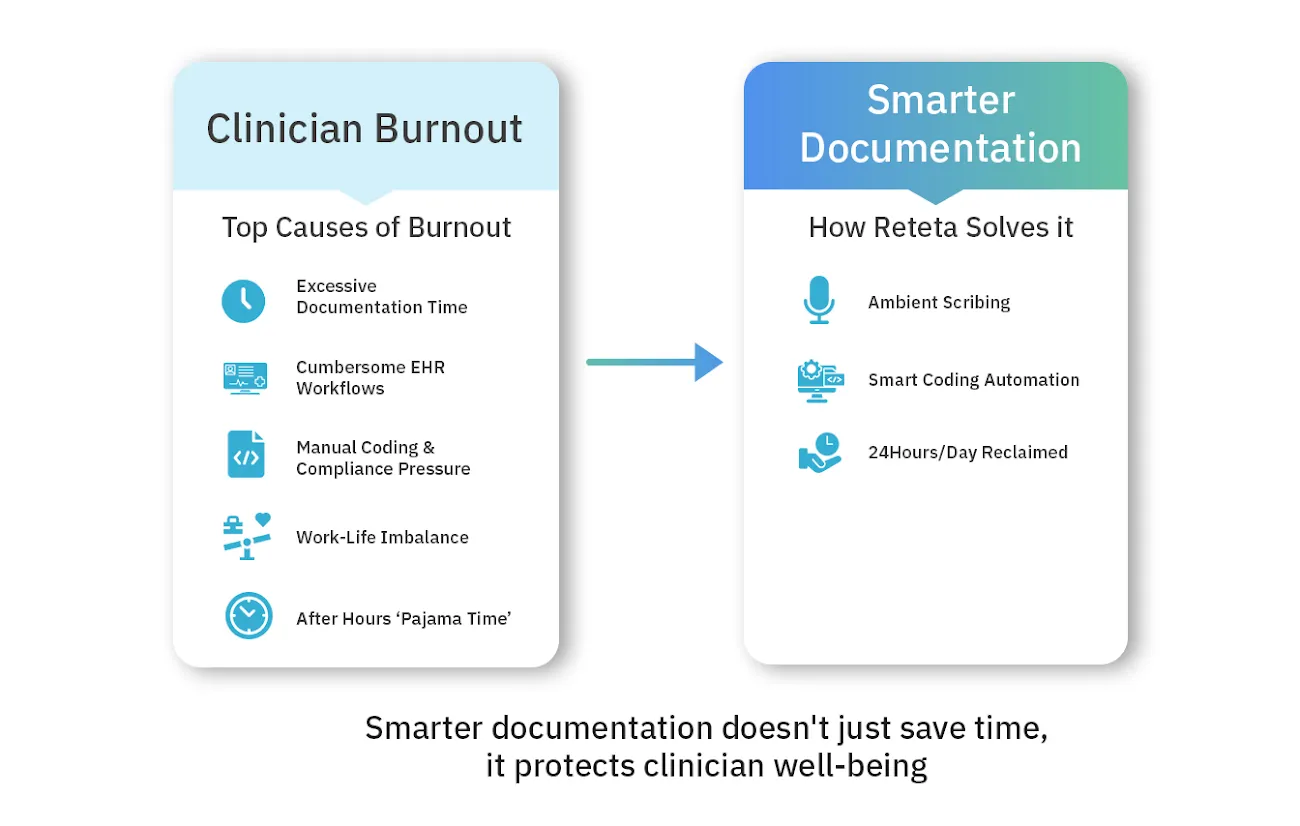
How Documentation Drives Clinician Burnout
When documentation takes more time than patient care, the impact is inevitable. Clinicians report exhaustion, emotional fatigue, and a loss of connection to their work. Studies show that administrative burden is consistently ranked among the top causes of physician burnout.
The consequences ripple outward:
- For clinicians: frustration, reduced job satisfaction, and loss of work-life balance.
- For patients: less engaged encounters and rushed interactions.
- For organizations: higher turnover, reduced productivity, and compromised care quality.
In short, documentation isn’t just paperwork, it’s one of the most powerful forces shaping the clinician experience.
Smarter Documentation is The Future
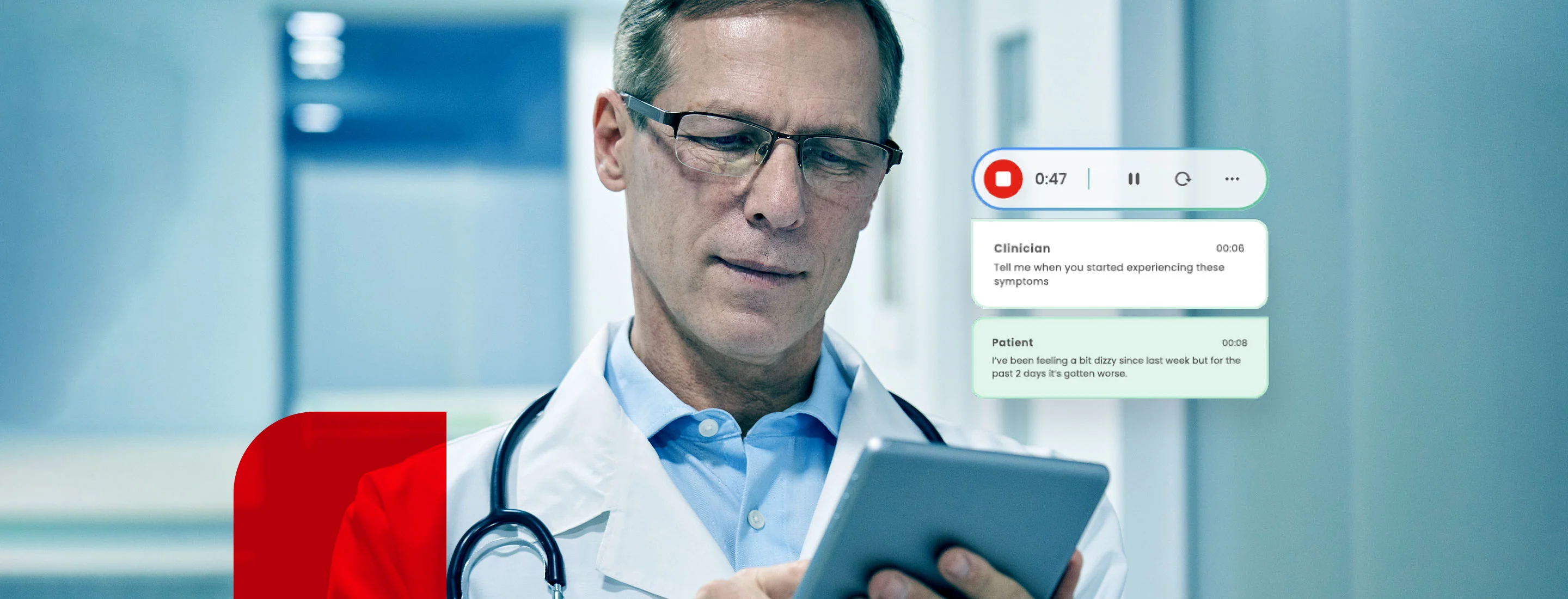
Documentation shouldn’t just record, it should understand. Smarter documentation organizes conversations into structured, compliant notes that are ready to use without extra effort. It works quietly in the background, easing the burden instead of adding to it.
Built with explainable AI at its core, Reteta captures clinician–patient interactions and turns them into clear SOAP notes, after-visit summaries, and referrals. The medical scribe also suggests accurate medical codes, flags documentation gaps in minutes, and integrates seamlessly with existing EHR systems. What makes it stand out is the way it adapts to clinicians’ workflows, allowing them to practice as they always have less paperwork and more time for patient care.
- Ambient Scribing: Reteta listens to patient–clinician conversations and generates structured SOAP notes, after-visit summaries, and referral letters automatically.
- Automated Coding: ICD-10 and the Current Procedural Terminology (CPT) codes are suggested in real time, reducing errors and eliminating manual coding backlogs.
- Seamless EHR Integration: Designed to work within existing electronic health record systems, enabling smooth adoption without disrupting clinician workflows.
From Features to Daily Reality: The Real Impact
The real power of smarter documentation isn’t in the technology itself. It’s in how it transforms daily life for clinicians.
Before Reteta: The last patient leaves, but the work stretches late into the night. Notes remain unfinished, coding is pushed to later, and fatigue deepens. The day doesn’t end when clinic hours do, it ends when the paperwork does.
After Reteta: Documentation is completed in real time during or right after the encounter. Coding suggestions appear automatically, ensuring accuracy and reducing errors. When the clinic closes, the work is done. Clinicians leave on time, free from the weight of unfinished charts.
This shift translates into three tangible outcomes:
- Time Savings: Health systems report that AI scribes save physicians more than an hour per day at the keyboard.
- Burnout Reduction: In a multi-site study, ambient documentation reduced reported burnout rates from over 50% to around 30% within months of adoption.
- ROI for Organizations: One system documented 15,700 hours of physician time saved in a single year. It is equivalent to nearly 1,800 workdays, while also improving coding accuracy and speeding up reimbursements.
Towards Sustainable Care
Clinician burnout isn’t a vague problem. It's a daily reality fueled by the documentation burden. But smarter documentation offers a clear path forward. With Reteta, clinicians don’t just save time - they regain balance, satisfaction, and focus on what matters most: patient care. Organizations don’t just streamline processes, they strengthen compliance, accelerate revenue, and build sustainable growth.
Smarter documentation isn’t about typing faster; it’s about transforming the way care is delivered. With Reteta, the shift is already happening: from endless paperwork to a future where clinicians leave on time, patients get better attention, and healthcare finally feels sustainable again.
Related Resources


Providers get reimbursed for all the services rendered with 85% increase in claim approval by Co-piloting with explainable AI scribe.
AI Medical Scribes: What They Are, How They Work, and Why You Need Them
Ready to unlock
clinical productivity through AI?
Experience the future of clinical documentation and coding. Request a personalized demo and see how Reteta can help your team reclaim time, reduce burnout, and improve care.
